In today’s fast-paced world, the traditional concept of primary care is undergoing a paradigm shift. With healthcare systems becoming increasingly complex and access to primary care physicians sometimes limited, emergency rooms (ERs) are stepping up to fill the gap as primary care providers for many individuals. This trend is reshaping the way we approach healthcare delivery, raising both opportunities and challenges. In this comprehensive exploration, we delve into the concept of emergency rooms as primary care providers, examining the reasons behind this shift, its implications for patients and healthcare systems, and potential strategies for optimizing this evolving model.
The Changing Landscape of Primary Care
Primary care serves as the cornerstone of healthcare systems, offering preventive services, managing chronic conditions, and addressing acute illnesses. Traditionally, primary care physicians have been the first point of contact for patients seeking non-emergency medical attention. However, several factors have contributed to the redefinition of primary care delivery:
Access Challenges: In many regions, access to primary care physicians is limited due to factors such as provider shortages, long wait times for appointments, and geographic barriers, especially in rural areas.
Cost Considerations: For individuals without health insurance or those with high deductibles, seeking care at an emergency room might seem more financially viable than visiting a primary care physician, especially if they anticipate needing extensive diagnostic tests or procedures.
24/7 Availability: Unlike primary care clinics, emergency rooms operate round-the-clock, making them accessible at any time of the day or night. This availability is particularly appealing for individuals with busy schedules or those experiencing health emergencies outside of regular office hours.
Scope of Services: Emergency rooms are equipped to handle a wide range of medical conditions, from minor injuries and infections to life-threatening emergencies. This comprehensive scope of services makes them a convenient option for patients seeking immediate care without the need for referrals or multiple appointments.
The Role of Emergency Rooms as Primary Care Providers
While emergency rooms have traditionally been reserved for critical and life-threatening conditions, they are increasingly serving as primary care providers for a significant portion of the population. This expanded role is driven by various factors, including patient preferences, systemic challenges, and evolving healthcare dynamics:
Patient Preferences: For many individuals, the emergency room represents a one-stop solution for their healthcare needs. They appreciate the convenience of walk-in appointments, short wait times, and the ability to receive comprehensive care under one roof.
Urgent Care Needs: Not all medical issues require immediate attention but still warrant prompt evaluation and treatment. Emergency rooms offer the flexibility to address urgent care needs without the constraints of appointment scheduling or limited office hours.
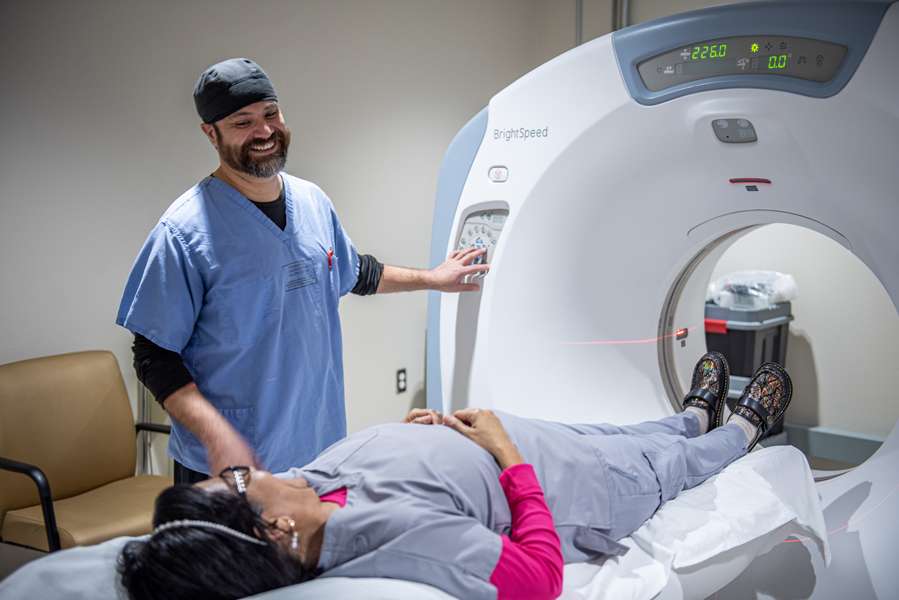
Diagnostic Capabilities: Emergency rooms are equipped with advanced diagnostic tools, including imaging technologies and laboratory facilities, allowing for rapid assessment and diagnosis of medical conditions. This diagnostic capacity is especially valuable for patients presenting with complex or undifferentiated symptoms.
Safety Net Function: For underserved populations or individuals without regular access to primary care, emergency rooms serve as a vital safety net, ensuring that they receive timely medical attention regardless of their insurance status or socioeconomic background.
Implications and Challenges
While the utilization of emergency rooms as primary care providers offers certain advantages, it also presents a set of challenges and implications that must be addressed:
Overcrowding and Wait Times: Increased reliance on emergency rooms for primary care can lead to overcrowding, longer wait times, and delays in treatment for patients with true emergencies. This strain on emergency resources can compromise the quality of care and patient satisfaction.
Resource Allocation: Emergency rooms are designed to handle acute and emergent conditions, necessitating specialized staffing, equipment, and infrastructure. Using them for primary care purposes may divert resources away from critical care services, potentially impacting patient outcomes.
Cost Burden: Emergency room visits are typically more expensive than primary care consultations, particularly for non-emergent conditions. Overreliance on emergency rooms for primary care can drive up healthcare costs and strain limited healthcare budgets.
Continuity of Care: Establishing long-term relationships and continuity of care are essential components of effective primary care. Emergency rooms, by nature, focus on immediate interventions rather than ongoing management, making it challenging to ensure consistent follow-up and coordination of care for chronic conditions.
Optimizing the Emergency Room Primary Care Model
Despite these challenges, there are several strategies that healthcare systems can implement to optimize the use of emergency rooms as primary care providers:
Enhanced Triage Systems: Implementing robust triage systems can help prioritize patients based on the acuity of their conditions, ensuring that those with true emergencies receive timely care while redirecting non-urgent cases to alternative care settings, such as urgent care centers or primary care clinics.
Integrated Care Models: Adopting integrated care models that facilitate collaboration between emergency departments, primary care practices, and specialty services can improve care coordination and ensure seamless transitions between different levels of care.
Telemedicine Solutions: Leveraging telemedicine technologies allows patients to access primary care services remotely, reducing the need for in-person emergency room visits for minor ailments or follow-up consultations.
Community Outreach and Education: Educating patients about appropriate healthcare utilization and the role of emergency rooms versus primary care providers can help alleviate unnecessary visits and promote the use of primary care for routine medical needs.
Conclusion
The evolving landscape of healthcare delivery necessitates a reevaluation of traditional models of primary care. While emergency rooms have historically served as critical hubs for acute care, their role as primary care providers is expanding in response to shifting patient preferences and systemic challenges. By recognizing the opportunities and addressing the challenges associated with this paradigm shift, healthcare systems can harness the potential of emergency rooms to deliver timely, accessible, and comprehensive primary care services to diverse patient populations. Effective collaboration, innovative solutions, and a patient-centered approach are essential in optimizing the emergency room as primary care model and ensuring high-quality healthcare delivery for all.