
Back pain is one of those problems that can sneak up on anyone, anytime. One day you’re fine, and the next, a sharp twinge or dull ache makes even simple movements a challenge. But not all back pain is created equal. A sprain or strain feels very different from the stabbing discomfort of a herniated disc. That’s why a one-size-fits-all approach rarely works. Tailored programs that address the specific cause and severity of your back pain can make all the difference in recovery and long-term relief.
Understanding the Spectrum of Back Pain
Sprains and Strains: The Common Culprits
Most back pain starts with a sprain or strain. These injuries involve overstretched or torn ligaments (sprains) or muscles and tendons (strains). They often happen during sudden movements, heavy lifting, or awkward twisting. The pain can range from mild soreness to sharp discomfort, and swelling or muscle spasms may follow.

Sprains and strains usually heal within a few weeks with proper care. Rest, ice, compression, and elevation—often abbreviated as RICE—are the first steps. But even within this category, the severity and location of the injury vary, requiring adjustments in treatment. For example, a mild lumbar strain might benefit from gentle stretching and movement early on, while a severe ligament sprain could require more rest and gradual rehabilitation. Additionally, incorporating physical therapy can significantly enhance recovery by focusing on strengthening the core muscles that support the spine, which can help prevent future injuries. Simple exercises such as pelvic tilts, bridges, and gentle back stretches can be effective in regaining strength and flexibility.
Disc Herniation: A Different Beast
A herniated disc occurs when the soft, gel-like center of a spinal disc pushes through a tear in its tougher exterior. This can irritate nearby nerves, causing pain, numbness, or weakness that radiates down the legs or arms. Unlike sprains and strains, disc herniations often involve nerve involvement, making the pain more complex.
Because of the nerve component, herniated discs usually demand a more nuanced approach. Treatments might include physical therapy focused on nerve mobilization, anti-inflammatory medications, and sometimes injections. In severe cases, surgery becomes an option. But most people respond well to conservative, tailored programs designed to reduce nerve irritation and strengthen supporting muscles. Moreover, lifestyle modifications play a crucial role in managing disc herniation. Maintaining a healthy weight, practicing good posture, and engaging in regular low-impact exercises like swimming or walking can alleviate pressure on the spine and promote overall spinal health. Understanding the mechanics of proper lifting techniques and avoiding prolonged sitting can also significantly reduce the risk of aggravating an existing herniation or developing new issues in the future. For more support and expert guidance, visit Advanced Pain Relief Clinic MK.
Why Tailored Back-Pain Programs Matter
One Size Does Not Fit All
Imagine trying to fix a car with a single tool, regardless of whether it’s a flat tire or engine trouble. That’s what generic back-pain treatments feel like. Every back is unique, and every injury has its own story. Tailored programs take into account the type of injury, pain intensity, lifestyle, and even psychological factors like stress or anxiety, which can influence pain perception and recovery.
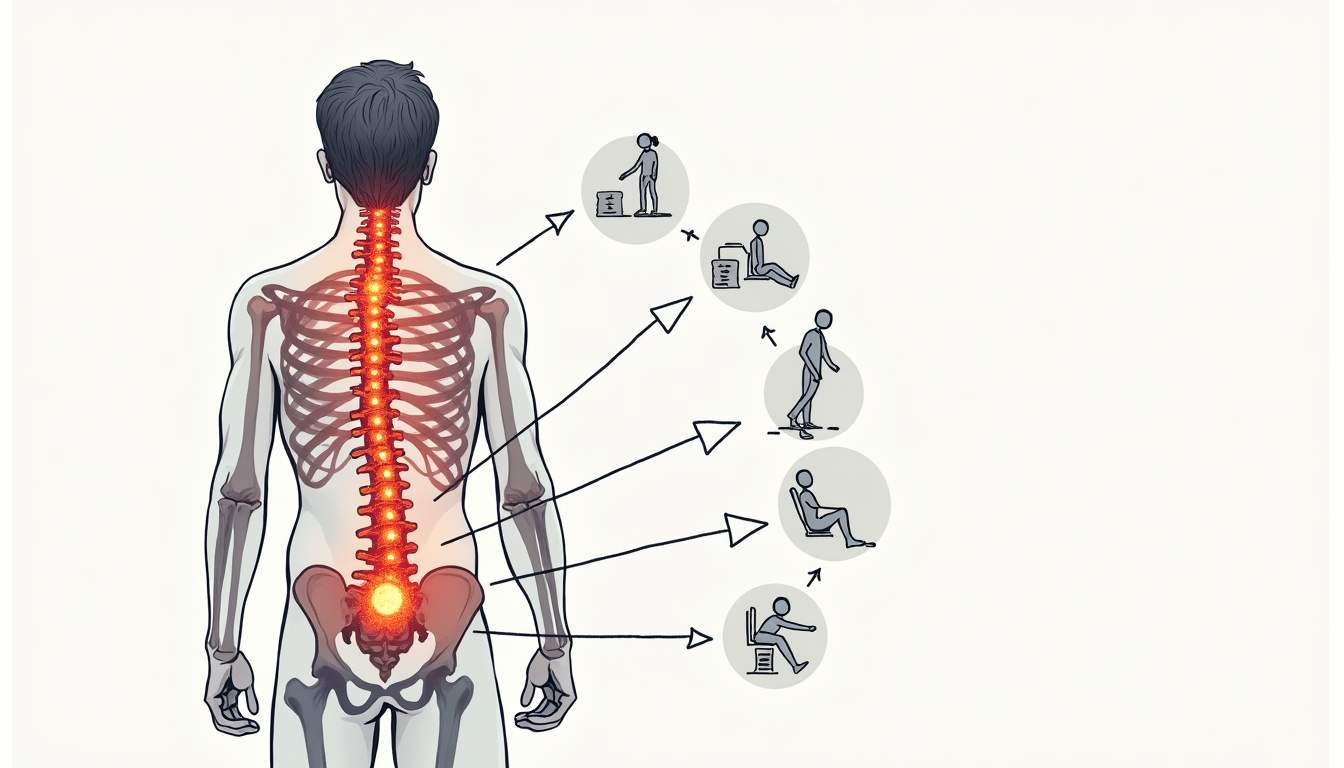
Customizing treatment means not only addressing the physical damage but also optimizing healing time and preventing future episodes. For example, someone with a mild strain from poor posture at work needs different interventions compared to an athlete with a herniated disc from a traumatic injury. Additionally, factors such as age, overall health, and even the patient’s personal goals play a critical role in shaping an effective treatment plan. A young professional may prioritize a quick return to the office, while a retiree might focus on regaining mobility for leisure activities. This nuanced understanding ensures that each individual receives a program that resonates with their specific needs and aspirations.
Improved Outcomes and Faster Recovery
When treatment aligns with the specific needs of the injury, recovery tends to be faster and more complete. Tailored programs often combine multiple approaches—manual therapy, exercise, education, and sometimes medication—to tackle pain from several angles. This multifaceted strategy not only addresses immediate pain relief but also empowers patients with knowledge and tools to manage their condition proactively.
Research consistently shows that patients engaged in personalized rehabilitation programs report less pain, improved function, and a higher quality of life. Plus, they’re less likely to develop chronic pain or require surgery down the line. The integration of technology, such as wearable devices that monitor movement and posture, further enhances these programs by providing real-time feedback and adjustments. This data-driven approach allows healthcare providers to fine-tune treatments as they progress, ensuring that patients are always on the most effective path to recovery. Moreover, the psychological support offered through tailored programs can foster a sense of community and accountability, encouraging patients to stay committed to their recovery journey and ultimately leading to more sustainable health outcomes.
Designing a Tailored Program for Sprains and Strains
Initial Assessment and Diagnosis
Before diving into treatment, a thorough assessment is essential. This includes a detailed history of how the injury occurred, the nature of the pain, and any aggravating or relieving factors. Physical examination focuses on range of motion, muscle strength, and identifying tender spots or spasms.
Imaging is rarely needed for simple sprains or strains unless symptoms persist or worsen. The goal is to classify the injury’s severity and rule out other causes. In some cases, a healthcare professional may utilize special tests to assess the integrity of ligaments or tendons, ensuring a comprehensive understanding of the injury. This thorough evaluation not only aids in diagnosis but also helps in crafting a personalized treatment plan that addresses the specific needs of the patient.
Early-Stage Management
In the first 48 to 72 hours, controlling inflammation and preventing further injury is key. Applying ice packs for 15-20 minutes every couple of hours can help reduce swelling and numb pain. Avoiding activities that exacerbate symptoms is important, but complete bed rest is discouraged as it can lead to stiffness and muscle weakness.
Gentle, pain-free movements should be encouraged early on to maintain flexibility. Over-the-counter pain relievers like NSAIDs can be useful but should be taken as directed. Additionally, incorporating compression wraps can provide support to the injured area, further minimizing swelling and promoting a sense of stability. Elevating the injured limb can also be beneficial, as it aids in reducing blood flow to the area, thereby decreasing inflammation and discomfort.
Rehabilitation and Strengthening
Once acute pain subsides, the focus shifts to restoring mobility and building strength. A physical therapist can guide through exercises targeting core muscles, which support the spine and reduce strain on injured tissues.
Stretching tight muscles, especially hamstrings and hip flexors, is crucial because tightness in these areas often contributes to back strain. Strengthening exercises should progress gradually, avoiding any movement that causes sharp pain. Incorporating balance and coordination exercises can also be advantageous, as they help improve overall stability and prevent future injuries. Techniques such as proprioceptive training, which enhances the body’s ability to sense its position in space, can be particularly effective in rehabilitating sprains and strains.
Posture and Ergonomics
Many sprains and strains stem from poor posture or repetitive stress. Tailored programs include education on proper body mechanics during daily activities and work. Ergonomic adjustments, such as chair support or workstation height, can prevent re-injury. Furthermore, individuals should be encouraged to take regular breaks during prolonged activities, especially those involving repetitive motions, to alleviate stress on muscles and joints. Simple practices like standing up to stretch or changing positions can significantly reduce the risk of developing chronic issues related to poor ergonomics.
In addition to physical adjustments, fostering awareness of body posture during various activities—such as lifting, sitting, or even walking—can empower individuals to make healthier choices. Workshops or seminars focusing on ergonomics and body mechanics can be beneficial, providing practical tips and techniques that individuals can implement in their daily routines. This holistic approach not only aids in recovery but also promotes long-term musculoskeletal health, ensuring that individuals are better equipped to manage their physical well-being in the future.
Addressing Disc Herniation with Precision
Comprehensive Evaluation
Disc herniation requires a more detailed evaluation because of nerve involvement. Along with physical examination, imaging like MRI often confirms the diagnosis and shows the extent of disc displacement.
Neurological tests assess reflexes, muscle strength, and sensation to determine which nerves are affected. This information guides the treatment plan.
Conservative Treatment First
Most herniated discs respond well to non-surgical approaches. A tailored program typically includes:
- Physical Therapy: Focused on exercises that reduce nerve pressure, improve spinal alignment, and strengthen core muscles.
- Medications: NSAIDs, muscle relaxants, or nerve pain medications as needed.
- Activity Modification: Avoiding heavy lifting or prolonged sitting, which can worsen symptoms.
- Education: Teaching proper body mechanics and pain management strategies.
Some patients benefit from epidural steroid injections to reduce inflammation around the nerve roots.
When Surgery Enters the Picture
Surgery is generally reserved for cases where conservative treatment fails after several weeks or when neurological deficits worsen. Procedures like microdiscectomy remove the herniated portion of the disc, relieving nerve pressure.
Even post-surgery, tailored rehabilitation is critical. It helps restore strength, flexibility, and prevents future problems.
Incorporating Lifestyle and Holistic Elements
Nutrition and Weight Management
Excess weight places additional stress on the spine. Tailored back-pain programs often include guidance on nutrition to support weight loss and reduce inflammation. Foods rich in antioxidants, omega-3 fatty acids, and vitamins D and C promote tissue healing.
Stress and Pain Connection
Stress can amplify pain perception and muscle tension. Mindfulness, relaxation techniques, and sometimes cognitive-behavioral therapy are valuable additions to a comprehensive program.
Sleep and Recovery
Quality sleep is essential for healing. Recommendations might include mattress adjustments, sleep position advice, and routines to improve rest.
Tracking Progress and Adjusting the Plan
Regular Monitoring
Back-pain recovery isn’t linear. Some days feel better, others worse. Regular check-ins with healthcare providers help track progress and tweak treatment as needed.
Patient Engagement
Active participation in the program is crucial. Patients who understand their condition and the rationale behind each step tend to stick with their plans and achieve better outcomes.
Preventing Recurrence
Once pain subsides, maintenance exercises and lifestyle changes keep the spine healthy. Tailored programs often transition into long-term wellness plans focused on flexibility, strength, and posture.
Final Thoughts
Back pain can be debilitating, but the right program tailored to the specific injury-from sprains and strains to disc herniations-can restore function and improve quality of life. Understanding the differences between these conditions and addressing them with personalized care makes all the difference. Whether it’s gentle stretching for a mild strain or targeted nerve mobilization for a herniated disc, a thoughtful, patient-centered approach paves the way to recovery.

Don’t settle for generic advice. Seek out programs that listen to your body, respect your unique needs, and guide you back to strength one step at a time.




